Eye Disease
Understanding Eye Disease: Causes, Types, and Treatments
Conjunctivitis
Conjunctivitis, commonly known as “pink eye,” is an inflammation or infection of the conjunctiva, which is the thin, transparent tissue that lines the inside of the eyelid and covers the white part of the eye. This condition can cause the eye to appear red or pink, hence the name.
Types of Conjunctivitis:
- Viral Conjunctivitis:
- Caused by viruses, often associated with the common cold.
- Highly contagious.
- Symptoms include watery discharge, itching, and sensitivity to light.
- Bacterial Conjunctivitis:
- Caused by bacteria like Staphylococcus or Streptococcus.
- Can lead to a thick, yellow-green discharge.
- May cause the eyelids to stick together, especially after sleep.
- Allergic Conjunctivitis:
- Triggered by allergens like pollen, dust, or pet dander.
- Not contagious.
- Symptoms include red eyes, itching, tearing, and swelling.
- Irritant Conjunctivitis:
- Caused by exposure to irritants like smoke, chlorine, or chemicals.
- Not contagious.
- Symptoms typically resolve once the irritant is removed.

Treatment:
- Conjunctivitis is usually a self-limiting disease, cold compresses and artificial tears may provide relief. It often resolves on its own in 1-2 weeks.
- . Maintain good hygiene, such as washing hands frequently.
- Avoid touching the eyes with unclean hands.
- Don’t share personal items like towels or eye makeup.
- If you wear contact lenses, follow proper care and cleaning instructions.
- Homeopathy has a natural and effective approach to soothe eyes ,and reduce inflammation and enhance eye immunity. Homeopathic med like belladonna and euphrasia is very helpful.
Dry Eye Syndrome
Dry Eye Syndrome (DES), also known as keratoconjunctivitis sicca, is a common condition where the eyes do not produce enough tears or the tears evaporate too quickly, leading to dryness, discomfort, and sometimes visual disturbances.

Symptoms of Dry Eye Syndrome:
- Stinging, burning, or scratchy sensation in the eyes.
- Sensitivity to light.
- Redness of the eyes.
- A feeling of having something in the eyes (foreign body sensation).
- Difficulty wearing contact lenses.
- Watery eyes, which is the body’s response to irritation from dry eyes.
- Blurred vision or eye fatigue.
Causes of Dry Eye Syndrome:
- Reduced Tear Production:
- Age: Tear production decreases with age.
- Medical conditions: Conditions like Sjögren’s syndrome, rheumatoid arthritis, or diabetes can reduce tear production.
- Medications: Certain medications like antihistamines, decongestants, antidepressants, and blood pressure medications can reduce tear production.
- Increased Tear Evaporation:
- Environmental factors: Wind, smoke, or dry air can increase tear evaporation.
- Blinking less often: This can occur when reading, driving, or staring at a computer screen for extended periods.
- Eyelid problems: Incomplete closure of the eyelids can lead to increased evaporation.
- Imbalance in Tear Composition:
- Tears are made up of three layers: oil, water, and mucus. An imbalance in these layers can cause dry eyes. For example, meibomian gland dysfunction can lead to a lack of the oil layer, causing tears to evaporate too quickly.
Prevention and Management:
- Maintain good eyelid hygiene.
- Blink regularly, especially during screen time.
- Stay hydrated.
- Wear sunglasses to protect against wind and sun.
- Home remedies for dry eyes with homeopathic medicine brings excellent results.
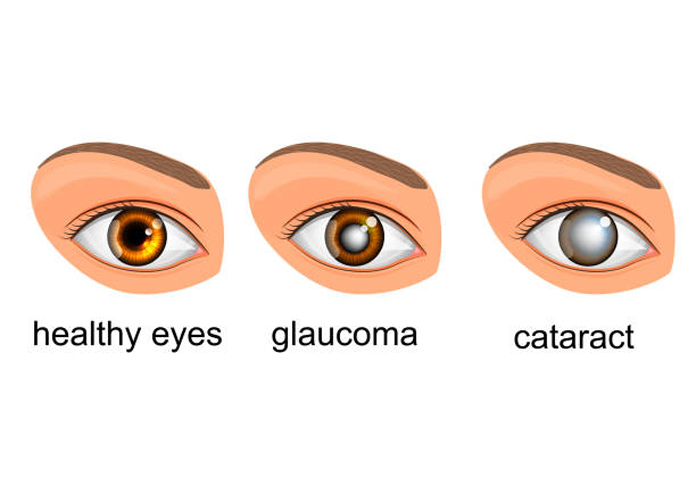
Glaucoma
Glaucoma is a group of eye conditions that damage the optic nerve, which is crucial for good vision. This damage is often caused by abnormally high pressure in the eye (intraocular pressure), though glaucoma can occur even with normal eye pressure. If left untreated, glaucoma can lead to irreversible vision loss and blindness.
Symptoms:
- Open-Angle Glaucoma:
- Often called the “silent thief of sight” because it progresses slowly and painlessly, with no noticeable symptoms until significant vision loss occurs.
- Gradual loss of peripheral (side) vision, leading to tunnel vision if untreated.
- Angle-Closure Glaucoma:
- Sudden, severe eye pain.
- Headache.
- Nausea and vomiting.
- Blurred vision.
- Halos around lights.
- Eye redness.
Types of Glaucoma:
- Open-Angle Glaucoma:
- Primary Open-Angle Glaucoma: The most common form, where the drainage angle formed by the cornea and iris remains open, but the trabecular meshwork becomes less efficient at draining fluid. This leads to gradual pressure buildup.
- Normal-Tension Glaucoma: The optic nerve is damaged even though the eye pressure is within the normal range. The cause is not well understood but may involve poor blood flow to the optic nerve.
- Angle-Closure Glaucoma (also called closed-angle glaucoma):
- Occurs when the iris bulges forward to narrow or block the drainage angle, leading to a sudden increase in eye pressure. This is a medical emergency and requires immediate treatment.
- Secondary Glaucoma:
- Develops as a complication of another condition, such as eye injury, inflammation, certain medications (like corticosteroids), or advanced cases of cataracts or diabetes.
- Congenital Glaucoma:
- A rare form that occurs in infants due to improper development of the eye’s drainage system before birth.
Prevention and Management:
- Regular eye exams, especially if you are at higher risk (age over 60, family history, African, Asian, or Hispanic descent, certain medical conditions like diabetes or high blood pressure).
- Protecting eyes from injury and maintaining overall eye health.
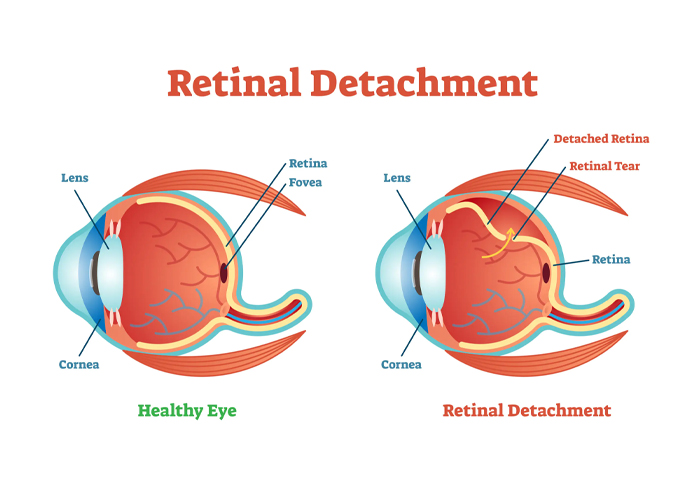
Retinal Detachment
Retinal detachment is a serious eye condition where the retina, a thin layer of tissue at the back of the eye responsible for capturing light and sending visual signals to the brain, separates from its normal position. This separation prevents the retina from functioning properly, leading to potential vision loss if not treated promptly.
Symptoms of Retinal Detachment:
- Sudden Appearance of Floaters: Small dark spots or lines that float across your field of vision.
- Flashes of Light: Seeing sudden flashes of light in one or both eyes.
- Blurred Vision: A sudden decrease in vision or the appearance of a shadow or curtain across part of your visual field.
- Peripheral Vision Loss: A gradual reduction in side vision.
Causes of Retinal Detachment:
- Rhegmatogenous Retinal Detachment:
- The most common type, caused by a tear or hole in the retina. This allows fluid from the eye to seep underneath the retina, causing it to lift away from the underlying tissue.
- Risk factors include aging, severe nearsightedness (myopia), previous eye surgery (like cataract removal), eye injury, or a family history of retinal detachment.
- Tractional Retinal Detachment:
- Occurs when scar tissue on the retina’s surface contracts, pulling the retina away from the back of the eye.
- Most commonly associated with diabetic retinopathy, a complication of diabetes that damages the blood vessels in the retina.
- Exudative Retinal Detachment:
- Occurs when fluid accumulates beneath the retina without any tears or holes, causing the retina to detach.
- Can be caused by inflammatory conditions, eye tumors, or diseases like age-related macular degeneration (AMD).
Prognosis:
- The success of retinal detachment treatment depends on how quickly the condition is diagnosed and treated.
- If treated promptly, many people regain most of their vision. However, if the detachment involves the central part of the retina (macula), some degree of permanent vision loss may occur.
Prevention and Management:
- Regular eye exams, especially if you are at high risk for retinal detachment.
- Immediate consultation with an eye specialist if you experience any symptoms like sudden floaters, flashes of light, or vision changes.
- Protect your eyes from injury by wearing safety goggles during activities that pose a risk of eye injury.
- Do not try Home remedies for dry eyes If you have retinal detachment.
Retinal detachment is a medical emergency. Prompt diagnosis and treatment are critical to preserving vision.
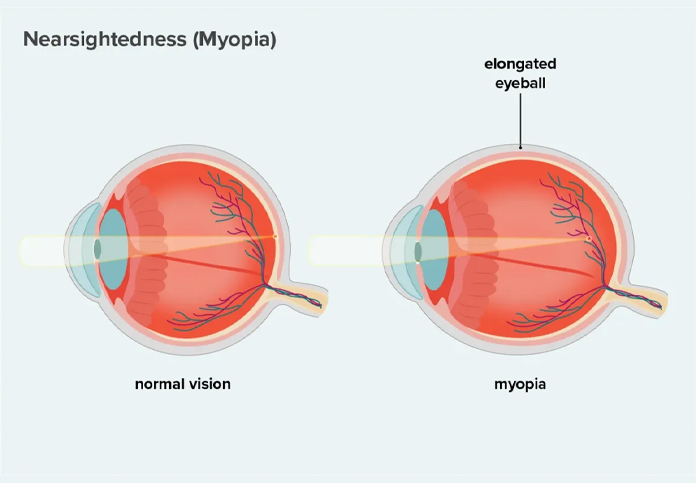
Myopic degeneration (also known as myopic macular degeneration or pathological myopia)
is a serious eye condition that occurs in people with high myopia (severe nearsightedness). In high myopia, the eye elongates more than normal, which stretches and thins the retina and other structures in the eye. This excessive elongation can lead to degenerative changes, particularly in the macula, the central part of the retina responsible for sharp vision.
Causes and Risk Factors:
- High Myopia: Typically defined as a refractive error greater than -6.00 diopters. The more elongated the eye, the greater the risk of degenerative changes.
- Genetics: A family history of high myopia or myopic degeneration increases the risk.
- Age: Although it can develop at any age, the risk increases as one ages.
- Ethnicity: Myopic degeneration is more common in East Asian populations, though it can occur in any ethnic group.
Pathological Changes:
- Thinning of the Retina: The stretching of the eye leads to thinning and weakening of the retinal layers.
- Choroidal Neovascularization (CNV): Abnormal blood vessels can grow beneath the retina, leading to leakage and scarring. This is similar to what happens in age-related macular degeneration (AMD).
- Lacquer Cracks: Small breaks in the Bruch’s membrane (a layer beneath the retina), which can lead to further complications like bleeding or CNV.
- Fuchs Spots: Areas of pigment deposition in the retina resulting from previous episodes of CNV.
Symptoms:
- Blurred or Distorted Vision: Central vision may become blurry or distorted, making it difficult to read, recognize faces, or perform tasks requiring fine vision.
- Scotomas: Dark or empty spots may appear in the central vision.
- Difficulty in Adjusting to Low Light: Vision may be particularly poor in dim lighting.
- Gradual Vision Loss: In severe cases, progressive vision loss can occur.
Management and Prevention:
- Regular Eye Exams: People with high myopia should have regular eye exams to monitor for signs of myopic degeneration.
- Monitoring Vision: Patients should be aware of changes in vision and report any new symptoms, such as sudden blurriness or distortion, to an eye care professional immediately.
- Protecting Vision: Wearing glasses or contact lenses that correct high myopia and using appropriate lighting for reading and other activities can help manage the condition.Home remedies for dry eyes
Prognosis:
- The prognosis varies depending on the severity of the degeneration and the success of treatment. While treatments can help manage the condition and slow progression, myopic degeneration often results in some degree of permanent vision loss, particularly in the central vision.Home remedies for dry eyes
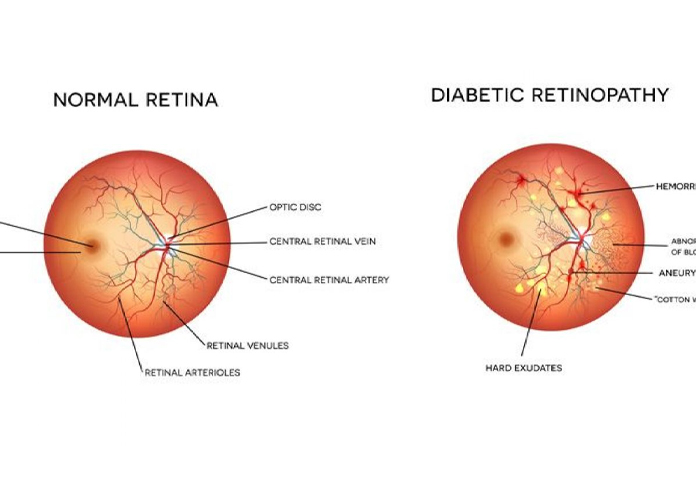
Diabetic retinopathy
Diabetic retinopathy is a diabetes-related eye condition that affects the blood vessels of the retina, the light-sensitive tissue at the back of the eye. Over time, high blood sugar levels can damage these blood vessels, leading to vision problems and, if left untreated, potential blindness.
Symptoms:
- Early Stages: Often asymptomatic, especially in the early stages (NPDR).
- As the Condition Progresses:
- Blurred or distorted vision.
- Floaters (dark spots or strings floating in your field of vision).
- Difficulty seeing at night.
- Loss of central vision (in DME).
- Sudden vision loss (in severe PDR or retinal detachment).
Stages of Diabetic Retinopathy:
- Non-Proliferative Diabetic Retinopathy (NPDR):
- Mild NPDR: Early stage where tiny blood vessels in the retina weaken and develop microaneurysms (small bulges that may leak fluid and blood).
- Moderate NPDR: As the disease progresses, some blood vessels that nourish the retina become blocked, leading to a buildup of fluids and more significant leakage.
- Severe NPDR: A large number of retinal blood vessels become blocked, depriving areas of the retina of their blood supply. This signals the retina to grow new blood vessels.
- Proliferative Diabetic Retinopathy (PDR):
- The most advanced stage, where the retina starts growing new, abnormal blood vessels (neovascularization). These vessels are fragile and prone to bleeding into the vitreous (the gel-like substance inside the eye), leading to more severe vision problems.
- Scar tissue from these vessels can cause retinal detachment.
- PDR can also lead to neovascular glaucoma, where abnormal blood vessels grow on the iris and block the eye’s drainage system, leading to increased eye pressure.
Diabetic Macular Edema (DME):
- Can occur at any stage of diabetic retinopathy.
- Involves swelling of the macula, the central part of the retina responsible for sharp, straight-ahead vision.
- DME is a common cause of vision loss in people with diabetic retinopathy.
Prevention and Management:
- Regular Eye Exams: People with diabetes should have a comprehensive dilated eye exam at least once a year, or more frequently if recommended by their eye care provider.
- Blood Sugar Management: Keeping blood sugar levels within target ranges can prevent or slow the progression of diabetic retinopathy.
- Blood Pressure and Cholesterol Control: Managing these can reduce the risk of developing or worsening retinopathy.
- Healthy Lifestyle: Maintaining a healthy diet, exercising regularly, and not smoking can help manage diabetes and reduce complications.Home remedies for dry eyes
Eye floaters
Eye floaters are small, shadowy shapes that drift across your field of vision. They can appear as dots, specks, squiggly lines, or cobwebs and are most noticeable when looking at something bright, like a blue sky or a white wall. While floaters are usually harmless, they can sometimes indicate a more serious eye condition.
Symptoms:
- Small Shapes in Your Vision: Floaters appear as dark spots, strings, or cobweb-like shapes that move when you move your eyes.
- Floaters Drift: They tend to drift out of the field of vision when you try to look at them directly.
- Increased Noticeability: They are more noticeable when looking at a plain, bright background.
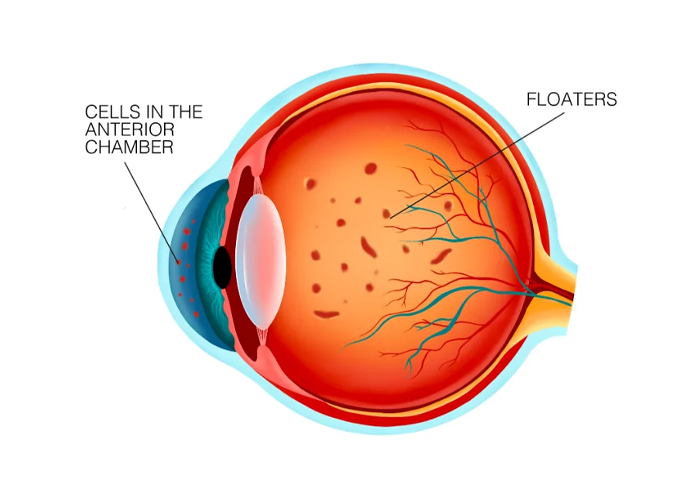
Causes of Eye Floaters:
- Aging:
- As you age, the vitreous (a gel-like substance inside the eye) begins to liquefy and shrink, causing tiny fibers within the vitreous to clump together. These clumps cast shadows on the retina, creating the appearance of floaters.
- Posterior Vitreous Detachment (PVD):
- Over time, the vitreous can pull away from the retina, leading to a condition called posterior vitreous detachment. PVD is common and usually harmless, but it can sometimes cause a sudden increase in floaters.
- Inflammation:
- Inflammation in the eye (uveitis) can cause inflammatory debris to enter the vitreous, which appears as floaters.
- Bleeding in the Eye:
- Bleeding into the vitreous, due to injury, diabetic retinopathy, or other conditions, can cause blood cells to appear as floaters.
- Retinal Tears or Detachments:
- A sudden increase in floaters, especially if accompanied by flashes of light or a loss of peripheral vision, can be a sign of a retinal tear or detachment, which is a medical emergency.
- Eye Surgery or Trauma:
- Certain eye surgeries or eye injuries can lead to the development of floaters.Home remedies for dry eyes
