Gastroenterology
Understanding Gastroenterology: Causes, Types, and Treatments
Gastritis
Gastritis is the inflammation of the stomach lining, which can occur suddenly (acute gastritis) or develop gradually over time (chronic gastritis). It can be caused by a variety of factors, including infections, prolonged use of certain medications, excessive alcohol consumption, and autoimmune conditions.Best Homeopathy Clinic In Bangalore
Types of Gastritis:
- Acute Gastritis:
- Onset: Sudden and severe.
- Symptoms: Often includes sharp or gnawing stomach pain, nausea, vomiting, and a feeling of fullness or bloating. In severe cases, there might be vomiting of blood or blood in the stool, which appears black and tarry.
- Chronic Gastritis:
- Onset: Develops slowly over time and may persist for months or years.
- Symptoms: Symptoms are often less severe but more persistent than in acute gastritis. They may include a dull ache in the upper abdomen, nausea, bloating, and a loss of appetite. Chronic gastritis can lead to complications like peptic ulcers or an increased risk of stomach cancer.Best Homeopathy Clinic In Bangalore

Causes:
- Helicobacter pylori Infection: The most common cause of gastritis worldwide. This bacterium can damage the stomach lining, leading to inflammation and, in some cases, ulcers or stomach cancer.
- NSAIDs: Long-term use of non steroidal anti-inflammatory drugs (e.g., ibuprofen, aspirin) can irritate the stomach lining.
- Alcohol: Excessive alcohol consumption can erode the stomach lining and increase inflammation.
- Stress: Severe physical stress, such as from surgery, injury, or severe illness, can lead to gastritis.
- Autoimmune Gastritis: In this condition, the body's immune system mistakenly attacks the cells of the stomach lining. This can lead to a decrease in stomach acid and vitamin B12 absorption, potentially causing pernicious anemia.
- Bile Reflux: A condition where bile flows back into the stomach from the small intestine, irritating the stomach lining.
- Other Infections and Diseases: Viral infections, such as cytomegalovirus, or other diseases, like Crohn's disease, can also cause gastritis.
Symptoms:
- Upper Abdominal Pain: Often described as burning, gnawing, or aching, located in the upper central part of the abdomen.
- Nausea: A common symptom that may lead to vomiting.
- Vomiting: Sometimes with blood, indicating severe inflammation or erosion of the stomach lining.
- Loss of Appetite: A decreased desire to eat, which can lead to weight loss.
- Bloating and Belching: A sensation of fullness or gas after eating.
- Indigestion: Discomfort or pain in the upper abdomen after eating.
Diagnosis:
- Medical History and Physical Examination: doctor will ask about your symptoms, diet, medication use, and lifestyle.
- Endoscopy: A thin, flexible tube with a camera (endoscope) is inserted down the throat to examine the stomach lining. Biopsies may be taken to check for inflammation, H. pylori infection, or other issues.
- Blood Tests: To check for anemia, H. pylori infection, or autoimmune conditions.
- Stool Test: To detect H. pylori infection or blood in the stool.
- Breath Test: A urea breath test can detect the presence of H. pylori.
Treatment: Homeopathy has a very good scope for gastric related complaints, we have seen 96% success rate, few of the remedies like robinia, nat phos, nux vomica is really helpful, further constitution approach based on physical mental emotional modalities are helpful to eradicate the problem with heart burn,bloating and discomfort,it improves digestion and nutrient absorbtion.
Complications:
- Peptic Ulcers: Open sores that develop on the stomach lining or the upper part of the small intestine.
- Anemia: Chronic gastritis can lead to anemia due to bleeding or impaired absorption of vitamin B12.
- Stomach Cancer: Chronic gastritis, especially when caused by H. pylori infection or autoimmune disorders, can increase the risk of developing gastric cancer.
Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a common, chronic gastrointestinal disorder that affects the large intestine (colon). It is characterized by a group of symptoms that occur together, including abdominal pain, bloating, and changes in bowel habits, such as diarrhea, constipation, or alternating between the two. IBS is a functional disorder, meaning that it involves a problem with how the gut works, but it does not cause structural damage to the intestines.Best Homeopathy Clinic In Bangalore
Types of IBS:
- IBS with Constipation (IBS-C):
- Symptoms: Predominantly hard or lumpy stools with infrequent bowel movements, often accompanied by abdominal discomfort or pain.
- IBS with Diarrhea (IBS-D):
- Symptoms: Frequent loose or watery stools, urgency to have bowel movements, and abdominal discomfort or pain.
- IBS with Mixed Bowel Habits (IBS-M):
- Symptoms: Alternating between constipation and diarrhea, with both types of stools occurring at least a quarter of the time.
- IBS Unclassified (IBS-U):
- Symptoms: Symptoms of IBS that do not fit into the above categories.Best Homeopathy Clinic In Bangalore
Causes:
The exact cause of IBS is unknown, but several factors may contribute to its development:
- Gut-Brain Interaction: Abnormalities in the communication between the brain and the gastrointestinal tract can affect how the intestines function.
- Gut Motility: Abnormal movement of the intestines, either too slow (leading to constipation) or too fast (leading to diarrhea), can cause symptoms.
- Gut Sensitivity: Increased sensitivity of the gut to pain or discomfort may lead to heightened perception of normal digestive processes.
- Inflammation: Low-grade inflammation in the intestines may play a role in some cases of IBS.
- Gut Microbiota: An imbalance in the gut's bacterial composition may contribute to symptoms.
- Infections: Some people develop IBS after a severe gastrointestinal infection, known as post-infectious IBS.
Symptoms:
- Abdominal Pain or Cramping: Typically located in the lower abdomen and relieved by passing stool.
- Bloating: A sensation of fullness or swelling in the abdomen.
- Changes in Bowel Habits: Including diarrhea, constipation, or alternating between the two.
- Mucus in the Stool: Some people with IBS notice mucus in their stool.
- Gas and Flatulence: Increased passing of gas.
- Fatigue and Sleep Disturbances: Often associated with IBS due to chronic discomfort and stress.
- :
Treatment:
Treatment for IBS is aimed at relieving symptoms and may include lifestyle changes, dietary adjustments, and medications.
- Dietary Changes:
- Low FODMAP Diet: A diet low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, which are poorly absorbed carbohydrates that can trigger IBS symptoms.
- Fiber: Soluble fiber supplements (e.g., psyllium) can help with constipation-predominant IBS. However, insoluble fiber may worsen symptoms in some people.
- Avoiding Trigger Foods: Spicy foods, caffeine, alcohol, and certain fats can trigger symptoms.
- Small, Frequent Meals: Eating smaller portions more frequently may help reduce symptoms.
- Medications:Homeopathic medicines like nux vom, ars alb, aloes are helpful, to further go to the deeper evaluation with constitution approach to balance the mental emotional modalities.very good success rate of 96% in ibs patients.
- Stress Management:
- Cognitive Behavioural Therapy (CBT): To help manage stress and anxiety, which can exacerbate IBS symptoms.
- Relaxation Techniques: Such as deep breathing exercises, meditation, and yoga.
- Physical Activity:
- Regular exercise can help reduce stress, improve gut motility, and alleviate symptoms.
Crohn's Disease
Crohn’s disease is a type of chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. However, it most commonly affects the end of the small intestine (the ileum) and the beginning of the colon. Crohn’s disease causes inflammation, which can lead to symptoms like severe abdominal pain, diarrhea, fatigue, weight loss, and malnutrition. The inflammation can affect different layers of the bowel wall and may cause complications such as strictures (narrowing of the bowel), fistulas (abnormal connections between organs), and abscesses (pockets of infection).Best Homeopathy Clinic In Bangalore
Causes:
The exact cause of Crohn’s disease is unknown, but it is thought to involve a combination of factors:
- Genetic Predisposition: People with a family history of Crohn’s disease are at a higher risk, suggesting a genetic component.
- Immune System Dysfunction: Crohn’s disease is thought to be an autoimmune disorder, where the body’s immune system mistakenly attacks the GI tract, leading to inflammation.
- Environmental Factors: Factors such as diet, smoking, and exposure to certain bacteria or viruses may trigger or exacerbate the condition.
- Microbiome Imbalance: An imbalance in the gut bacteria may contribute to the development of Crohn’s disease.Best Homeopathy Clinic In Bangalore

Symptoms:
Symptoms of Crohn's disease can vary depending on the part of the GI tract affected and the severity of the inflammation. Common symptoms include:
- Abdominal Pain and Cramping: Often in the lower right side of the abdomen, but can occur anywhere.
- Chronic Diarrhea: Often with blood or mucus.
- Weight Loss: Due to malabsorption of nutrients and loss of appetite.
- Fatigue: A common symptom due to chronic inflammation, anemia, or malnutrition.
- Fever: Low-grade fevers may occur during flare-ups.
- Mouth Sores: Ulcers in the mouth may develop during active disease.
- Rectal Bleeding: Blood in the stool due to inflammation or ulcers.
- Anemia: Caused by chronic blood loss or malabsorption of iron or vitamin B12.
- Perianal Disease: Inflammation around the anus, leading to pain, swelling, or abscesses.
Treatment:
- Homeopathic management gives symptomatic relief initially, reducing inflammation and promoting overall well being.constitutional approach is very important than a symptomatic relief. Remedies like merc, sulphur, nux vom are very helpful.
- Lifestyle and Dietary Management:
- Dietary Adjustments: Eating smaller, more frequent meals, avoiding high-fiber foods during flare-ups, and staying hydrated can help manage symptoms.
- Nutritional Supplements: Iron, calcium, vitamin D, and vitamin B12 supplements may be necessary due to malabsorption.
- Smoking Cessation: Smoking is known to worsen Crohn's disease, so quitting smoking is highly recommended.
- Stress Management: Stress can exacerbate symptoms, so stress reduction techniques like meditation, exercise, and counseling can be beneficial.
Ulcerative colitis
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon (large intestine) and the rectum. It causes inflammation and ulcers (sores) on the inner lining of the colon, leading to symptoms such as abdominal pain, diarrhea, and rectal bleeding. Unlike Crohn’s disease, which can affect any part of the gastrointestinal tract, ulcerative colitis is limited to the colon and always involves the rectum.Best Homeopathy Clinic In Bangalore
Causes:
The exact cause of ulcerative colitis is unknown, but it is thought to result from a combination of factors:
- Immune System Dysfunction: An abnormal immune response causes the immune system to attack the cells of the colon lining, leading to inflammation.
- Genetics: Family history plays a role, suggesting a genetic predisposition to the disease.
- Environmental Factors: Factors such as diet, stress, and certain infections may trigger or exacerbate the condition.Best Homeopathy Clinic In Bangalore
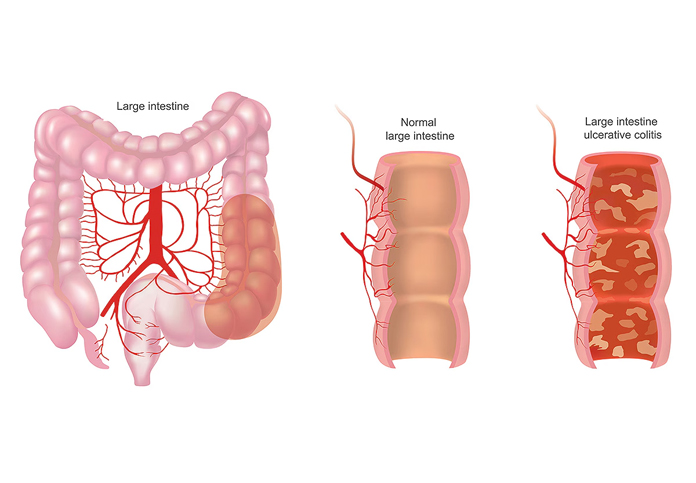
Types of Ulcerative Colitis:
Ulcerative colitis can be classified based on the extent of the colon affected:
- Ulcerative Proctitis:
- Affected Area: Involves only the rectum.
- Symptoms: Mild rectal bleeding, urgency to defecate, and rectal pain.
- Proctosigmoiditis:
- Affected Area: Involves the rectum and the sigmoid colon (the lower end of the colon).
- Symptoms: Bloody diarrhea, abdominal cramps, and urgency to defecate.
- Left-Sided Colitis:
- Affected Area: Involves the rectum, sigmoid colon, and descending colon (extends up the left side of the abdomen).
- Symptoms: Bloody diarrhea, abdominal pain on the left side, weight loss, and loss of appetite.
- Pancolitis:
- Affected Area: Involves the entire colon.
- Symptoms: Severe bloody diarrhea, abdominal cramps, fatigue, weight loss, and fever.
- Acute Severe Ulcerative Colitis:
- Affected Area: A severe and rare form of the disease that affects the entire colon.
- Symptoms: Severe pain, heavy bleeding, fever, and an inability to eat. This form of UC can be life-threatening and requires immediate medical attention.
Symptoms:
Symptoms of ulcerative colitis can vary depending on the severity and extent of the inflammation:
- Diarrhea: Often with blood or pus.
- Abdominal Pain and Cramping: Typically located in the lower left side of the abdomen.
- Rectal Bleeding: Blood may be noticed in the stool or passed alone.
- Urgency to Defecate: A frequent and sudden need to have a bowel movement, sometimes accompanied by a sensation of incomplete evacuation.
- Weight Loss: Due to reduced appetite, malnutrition, or both.
- Fatigue: Often related to chronic inflammation, anemia, or malnutrition.
- Fever: In severe cases or during flare-ups.
Treatment:
The treatment of ulcerative colitis aims to reduce inflammation, manage symptoms, and achieve and maintain remission. Treatment options include medications, lifestyle changes, Homeopathic medicines like nux vom, ars, merc sol is very helpful.
- Lifestyle and Dietary Management:
- Dietary Adjustments: Eating smaller, more frequent meals, avoiding high-fiber foods during flare-ups, and avoiding foods that trigger symptoms can help manage UC.
- Nutritional Supplements: Supplementation with vitamins and minerals (e.g., iron, calcium, vitamin D) may be necessary due to malabsorption or dietary restrictions.
- Stress Management: Stress can exacerbate symptoms, so stress-reduction techniques such as yoga, meditation, and regular exercise are beneficial.
Gallstones
Gallstones, also known as cholelithiasis, are solid particles that form in the gallbladder, a small organ located beneath the liver. The gallbladder stores bile, a digestive fluid produced by the liver that helps break down fats. Gallstones can vary in size and may be as small as a grain of sand or as large as a golf ball. Some people with gallstones may experience no symptoms (asymptomatic), while others may develop severe pain or complications.if you are looking for Best Homeopathy Clinic In Bangalore health global homeopathy is the best.
Types of Gallstones:
There are two main types of gallstones:
- Cholesterol Gallstones:
- Composition: Made primarily of hardened cholesterol.
- Appearance: Usually yellow-green in color.
- Prevalence: The most common type, accounting for about 80% of gallstones.
- Pigment Gallstones:
- Composition: Made of bilirubin, a substance produced from the breakdown of red blood cells.
- Appearance: Dark brown or black in color.
- Prevalence: Less common, often associated with certain medical conditions, such as liver cirrhosis, biliary tract infections, or sickle cell anemia.Best Homeopathy Clinic In Bangalore
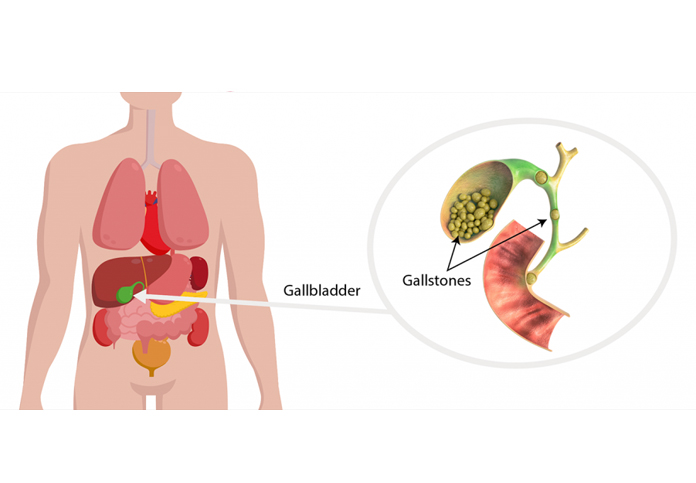
Causes:
Gallstones form when there is an imbalance in the substances that make up bile:
- Excess Cholesterol in Bile: Normally, bile contains enough chemicals to dissolve the cholesterol excreted by the liver. However, if the liver excretes more cholesterol than bile can dissolve, the excess cholesterol may crystallize and eventually form gallstones.
- Excess Bilirubin in Bile: Certain medical conditions can cause the liver to produce too much bilirubin, which can lead to the formation of pigment gallstones.
- Gallbladder Dysfunction: If the gallbladder doesn't empty completely or frequently enough, bile can become concentrated, leading to the formation of gallstones.
Risk Factors:
Several factors can increase the risk of developing gallstones:
- Gender: Women are more likely to develop gallstones than men.
- Age: The risk increases with age, particularly after age 40.
- Obesity: Being overweight is a significant risk factor due to increased cholesterol levels in bile.
- Rapid Weight Loss: Losing weight quickly can increase the risk of gallstones because of rapid changes in bile composition.
- Pregnancy: Hormonal changes during pregnancy can increase cholesterol levels in bile and decrease gallbladder motility.
- Diet: A diet high in fat and cholesterol and low in fiber increases the risk of gallstones.
- Family History: Genetics may play a role in the likelihood of developing gallstones.
- Certain Medical Conditions: Conditions like diabetes, cirrhosis, and certain blood disorders can increase the risk.
- Medications: Certain medications, such as hormone replacement therapy or cholesterol-lowering drugs, can increase the risk of gallstones.
Symptoms:
Gallstones may cause no symptoms at all (asymptomatic gallstones), but when they do, the symptoms can include:
- Biliary Colic: Sudden, intense pain in the upper right abdomen or center of the abdomen, often occurring after eating a fatty meal. The pain may radiate to the back or right shoulder blade and can last from a few minutes to several hours.
- Nausea and Vomiting: Often accompany the pain.
- Jaundice: Yellowing of the skin and eyes if a gallstone blocks the bile duct, leading to bile buildup in the liver.
- Fever and Chills: May indicate an infection in the bile ducts or gallbladder.
- Dark Urine and Pale Stools: Caused by bile flow obstruction.
Treatment;homeopathic medicines like chelidonium, cardus mur,beri beri vulgaris, lyco is helpful for dissolving small gall stones ,reduce pain and inflammation,improve bile flow and digestion,enhance overall wellbeing.
Benefits of homeopathy for gall stones non invasive and pain free,no risk of surgery or complications
Lifestyle and Dietary Management:
- Dietary Changes: Eating a diet low in fat and cholesterol and high in fiber can help prevent the formation of gallstones.
- Maintaining a Healthy Weight: Gradual weight loss can reduce the risk of gallstones.
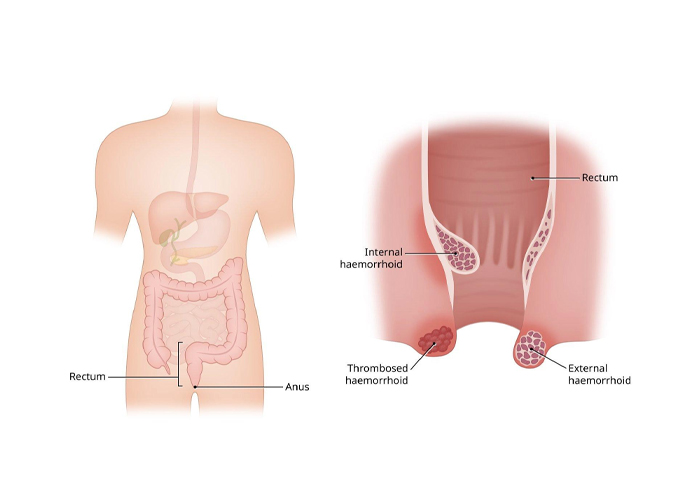
Piles
Piles, also known as hemorrhoids, are swollen and inflamed veins in the rectum and anus that cause discomfort and bleeding. Hemorrhoids can occur inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids). They are a common condition, especially among adults, and can range from mild to severe.if you are looking for Best Homeopathy Clinic In Bangalore health global homeopathy is the best
Types of Hemorrhoids:
- Internal Hemorrhoids:
- Location: Inside the rectum.
- Symptoms: Generally painless but may cause bleeding during bowel movements. Larger internal hemorrhoids may protrude outside the anus (prolapsed hemorrhoids) and can be painful.
- External Hemorrhoids:
- Location: Under the skin around the anus.
- Symptoms: Can cause itching, pain, and swelling around the anus. If a blood clot forms inside an external hemorrhoid (thrombosed hemorrhoid), it can be extremely painful.
Causes:
Hemorrhoids develop due to increased pressure in the lower rectum, which can cause the veins to stretch and swell. Common causes include:
- Straining During Bowel Movements: Often due to constipation or diarrhea.
- Sitting for Long Periods: Especially on the toilet.
- Chronic Constipation or Diarrhea: Both can lead to increased pressure in the rectal veins.
- Obesity: Increased abdominal pressure can contribute to the development of hemorrhoids.
- Pregnancy: The growing uterus puts pressure on the veins in the lower abdomen, which can lead to hemorrhoids.
- Low-Fiber Diet: Can cause constipation and straining, which contribute to hemorrhoid formation.
- Heavy Lifting: Frequent heavy lifting can increase abdominal pressure.
- Aging: Tissues supporting the veins in the rectum and anus can weaken with age, making hemorrhoids more likely.
Symptoms:
Symptoms of hemorrhoids can vary depending on the type and severity, but common symptoms include:
- Rectal Bleeding: Bright red blood may be noticed on toilet paper, in the toilet bowl, or on the surface of the stool.
- Itching or Irritation: Around the anus.
- Pain or Discomfort: Especially with external hemorrhoids.
- Swelling Around the Anus: A lump near the anus, which may be sensitive or painful.
- Prolapsed Hemorrhoid: Internal hemorrhoids that have protruded through the anus can cause pain and discomfort.
Treatment:
Treatment for hemorrhoids depends on the severity of the symptoms. Many cases of hemorrhoids can be managed with life style changes and home treatments. While some of the homeopathic remedies like nux vom, aloes, are very helpful. Homeopathic med can help to reduce pain, itching and discomfort,shrink swollen hemorrhoids,improve bowel movements and digestion
- Home Remedies:
- High-Fiber Diet: Eating more fruits, vegetables, and whole grains can soften stool and make it easier to pass, reducing the need to strain.
- Hydration: Drinking plenty of water helps prevent constipation.
- Warm Sitz Baths: Sitting in a warm bath for 10-15 minutes several times a day, es pecially after bowel movements, can relieve pain and itching.
- Cold Compresses: Applying ice packs to the affected area can reduce swelling.
- Avoiding Straining: Avoid prolonged sitting on the toilet and straining during bowel movements.
- Eat a High-Fiber Diet: Incorporate plenty of fruits, vegetables, and whole grains to prevent constipation.
- Stay Hydrated: Drink enough water throughout the day.
- Exercise Regularly: Regular physical activity can help prevent constipation and reduce pressure on the veins.
- Avoid Straining: Don’t strain during bowel movements, and avoid sitting on the toilet for long periods.
- Maintain a Healthy Weight: Reducing excess weight can lower the risk of developing hemorrhoids.
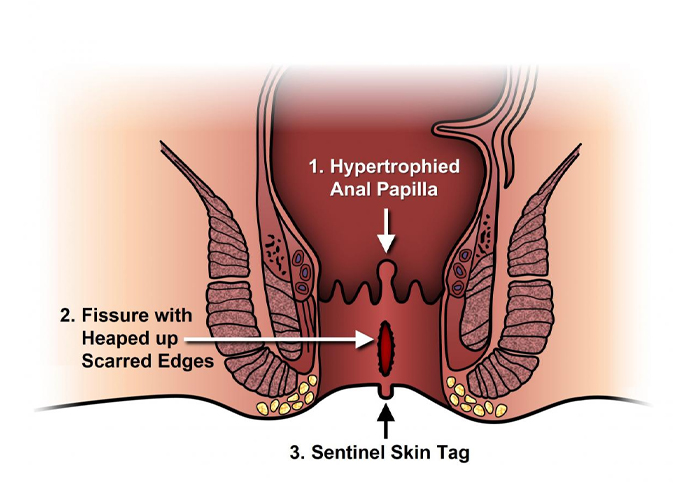
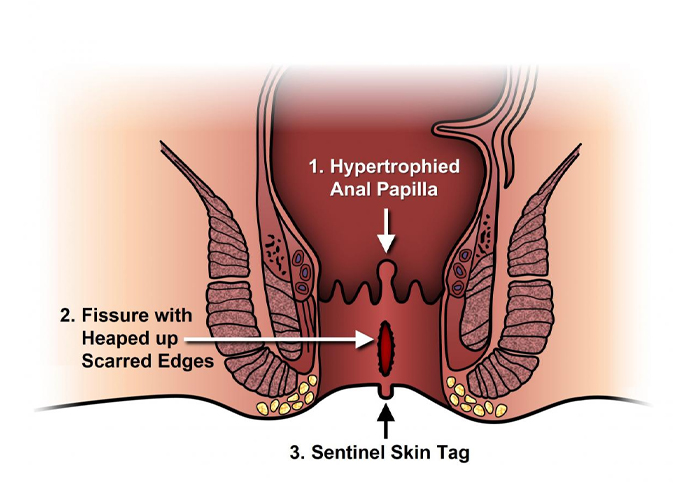
Fissure in Ano
A fissure in ano, commonly known as an anal fissure, is a small tear or crack in the lining of the anus, the opening through which stool passes. This condition can cause significant pain, bleeding, and discomfort during bowel movements. Anal fissures are a common condition and can affect people of all ages, though they are particularly common in infants and middle-aged adults.Best Homeopathy Clinic In Bangalore
Causes:
Anal fissures typically result from trauma to the anal canal. Common causes include:
- Constipation: Straining during bowel movements, passing large or hard stools, or experiencing prolonged constipation can cause the anal lining to tear.
- Diarrhea: Frequent loose stools can also lead to irritation and tearing of the anal canal.
- Childbirth: Women may develop fissures due to the strain of delivery.
- Anal Intercourse: This can also be a cause of anal fissures due to trauma to the anal tissue.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease can increase the risk of fissures due to chronic inflammation and diarrhea.
- Other Trauma: Inserting objects into the anus or aggressive wiping can cause fissures.
Symptoms:
The symptoms of an anal fissure are usually quite distinctive and can include:
- Pain During Bowel Movements: Sharp, burning, or severe pain during and after passing stool. This pain can last for several minutes to hours after a bowel movement.
- Bleeding: Bright red blood may be noticed on the toilet paper or in the stool. The bleeding is usually minimal.
- Itching or Irritation: Around the anus, often due to the presence of the fissure.
- Visible Tear: In some cases, the fissure may be visible near the anal opening.
- Spasm of the Anal Sphincter: This can contribute to the ongoing pain and difficulty in healing.
Types:
Anal fissures can be classified as:
- Acute Anal Fissures: Short-term fissures that usually heal on their own within a few weeks with conservative treatment.
- Chronic Anal Fissures: Fissures that persist for more than 6-8 weeks. They may require more intensive treatment, and often have a raised edge or a skin tag near the tear.
Treatment:
Treatment for anal fissures focuses on relieving symptoms and promoting healing. The approach depends on whether the fissure is acute or chronic. Homeopathic remedies like Rathania, nitric acid are helpful to reduce pain ,itching, discomfort, promote healing and tissue repair,improve bowel movements and digestion.
Prevention:
To prevent anal fissures or reduce the risk of recurrence:
- Avoid Straining: During bowel movements, try to avoid straining, which can cause or worsen fissures.
- Maintain Regular Bowel Habits: Regular bowel movements with soft, easy-to-pass stools can help prevent fissures. A diet rich in fiber and adequate fluid intake is key.
- Practice Good Anal Hygiene: Gentle cleaning after bowel movements can prevent irritation.
Fistula
A fistula is an abnormal connection or passageway that forms between two organs, or between an organ and the skin. It can occur in various parts of the body and can result from injury, infection, surgery, or certain medical conditions. Fistulas can be either congenital (present at birth) or acquired (developing later in life).Best Homeopathy Clinic In Bangalore
Causes:
Fistulas can develop from various underlying causes, including:
- Infections: Such as abscesses or chronic infections.
- Inflammatory Diseases: Conditions like Crohn’s disease or ulcerative colitis.
- Surgical Complications: Post-surgical wounds or complications.
- Trauma: Injury to the organs or surrounding tissues.
- Cancer: Tumors that erode through tissues and create abnormal connections.
- Radiation Therapy: Can lead to tissue damage and fistula formation.
Types of Fistulas:
- Anal Fistula:
- Location: Between the anal canal or rectum and the skin around the anus.
- Causes: Often results from an infection in the anal glands that forms an abscess. The abscess can then create a tunnel to the skin.
- Symptoms: Pain around the anus, swelling, discharge of pus or blood from the opening, and irritation.
- Rectovaginal Fistula:
- Location: Between the rectum and the vagina.
- Causes: Often due to childbirth complications, surgery, or inflammatory bowel disease.
- Symptoms: Unpleasant discharge of fecal matter from the vagina, frequent vaginal infections, and discomfort.
- Ureterovaginal Fistula:
- Location: Between the ureter (the tube connecting the kidney to the bladder) and the vagina.
- Causes: Can occur after surgery, trauma, or radiation therapy.
- Symptoms: Abnormal leakage of urine from the vagina, frequent urinary tract infections, and discomfort.
- Arteriovenous Fistula:
- Location: Between an artery and a vein.
- Causes: Can be congenital or result from trauma or surgery, often used intentionally in medical procedures like dialysis.
- Symptoms: May not always cause symptoms, but can lead to swelling, pain, or a pulsating mass in the area.
- Enteric Fistula:
- Location: Between the intestine and another organ or the skin.
- Causes: Often due to surgery, trauma, or inflammatory bowel disease.
- Symptoms: Leakage of intestinal contents, malnutrition, and dehydration.
Symptoms:
The symptoms of a fistula vary depending on its location and the organs involved. Common symptoms include:
- Discharge: Fluid, pus, or blood coming from an abnormal opening.
- Pain and Discomfort: Around the area of the fistula or where the connection occurs.
- Swelling: In the area around the fistula.
- Infections: Frequent or persistent infections at the site of the fistula.
- Urinary or Fecal Leakage: Depending on the location, leakage of urine or stool from an abnormal opening.
Treatment; Homeopathic medicines are helpful for promoting healing, reducing inflammation and addressing underlying cause without side effects. some commonly used medicines are silicea, hepar sulph , myristica.
Dietary advise and life style modification is very important.
