Female Sexual Diseases
Understanding Female Sexual Diseases: Causes, Types, and Treatments
Female Infertility
Female infertility refers to the inability of a woman to conceive after a year of regular, unprotected sexual intercourse. It can be due to a variety of factors affecting the reproductive system, hormonal balance, or overall health.
Symptoms:
- Irregular or Absent Menstrual Cycles: Difficulty in predicting ovulation or having infrequent periods.
- Painful Periods: Severe menstrual cramps or pelvic pain, which could be indicative of endometriosis or other conditions.
- Unexplained Weight Gain or Loss: Significant changes in weight can affect fertility.
- Hormonal Imbalances: Symptoms such as excessive hair growth, acne, or changes in skin texture.

Causes of Female Infertility:
- Ovulatory Disorders:
- Polycystic Ovary Syndrome (PCOS): A common hormonal disorder that can cause irregular or absent ovulation.
- Hypothalamic Amenorrhea: Disruption in the hormones produced by the hypothalamus can lead to irregular or absent menstrual cycles.
- Premature Ovarian Insufficiency: Early menopause or reduced ovarian function before age 40.
- Fallopian Tube Blockage:
- Pelvic Inflammatory Disease (PID): Infections of the reproductive organs can cause scarring and blockages in the fallopian tubes.
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, potentially leading to blockages or adhesions.
- Uterine Conditions:
- Fibroids: Noncancerous growths in the uterus that can interfere with implantation.
- Polyps: Growths on the lining of the uterus that can affect implantation.
- Congenital Abnormalities: Structural abnormalities of the uterus, such as a septum or abnormal shape.
- Hormonal Imbalances:
- Thyroid Disorders: Both hyperthyroidism and hypothyroidism can affect menstrual cycles and fertility.
- Hyperprolactinemia: Elevated levels of prolactin hormone can interfere with ovulation.
- Age:
- Female fertility declines with age, particularly after age 35, due to a decrease in the number and quality of eggs.
- Lifestyle Factors:
- Obesity: Excess weight can affect hormone levels and ovulation.
- Underweight: Being underweight can lead to irregular or absent menstrual cycles.
- Smoking: Can reduce fertility by affecting the fallopian tubes and eggs.
- Alcohol and Drug Use: Excessive use can impair fertility.
- Immune System Disorders:
- Autoimmune Diseases: Conditions such as lupus or antiphospholipid syndrome can affect fertility.
- Genetic Conditions:
- Turner Syndrome: A chromosomal disorder where a female is missing part or all of one of her X chromosomes.
- Fragile X Syndrome: A genetic condition that can cause premature ovarian failure.
- Environmental and Occupational Factors:
- Exposure to toxins, chemicals, and radiation can impact fertility.
Symptoms:
- Irregular or Absent Menstrual Cycles: Difficulty in predicting ovulation or having infrequent periods.
- Painful Periods: Severe menstrual cramps or pelvic pain, which could be indicative of endometriosis or other conditions.
- Unexplained Weight Gain or Loss: Significant changes in weight can affect fertility.
- Hormonal Imbalances: Symptoms such as excessive hair growth, acne, or changes in skin texture.
Diagnosis:
- Medical History and Physical Exam: Assessment of menstrual cycles, sexual history, and general health.
- Ovulation Testing: Monitoring basal body temperature or using ovulation predictor kits to determine if ovulation is occurring.
- Hormone Testing: Blood tests to check levels of reproductive hormones, thyroid hormones, and prolactin.
- Imaging Tests:
- Ultrasound: Used to evaluate the ovaries, uterus, and fallopian tubes for abnormalities.
- Hysterosalpingography (HSG): An X-ray of the uterus and fallopian tubes after injecting a contrast dye, used to identify blockages.
- Sonohysterography: A type of ultrasound where a saline solution is injected into the uterus to better visualize its structure.
- Laparoscopy: A minimally invasive surgery that allows direct visualization of the pelvic organs and can be used to diagnose conditions like endometriosis or pelvic adhesions.
- Endometrial Biopsy: A sample of the uterine lining is taken to check for abnormal cells or other issues.
Treatment:
- Lifestyle Changes:
- Healthy Diet and Exercise: Maintaining a healthy weight and balanced diet can improve fertility.
- Stress Management: Reducing stress through relaxation techniques or counseling can improve overall health and fertility.
- Smoking Cessation: Quitting smoking can enhance fertility and improve reproductive health.
- Homeopathic medicines like nat mur, sepia, lachesis,calc carb are very effective in gentle way to treat infertility and many other med are applied depending on the cause.
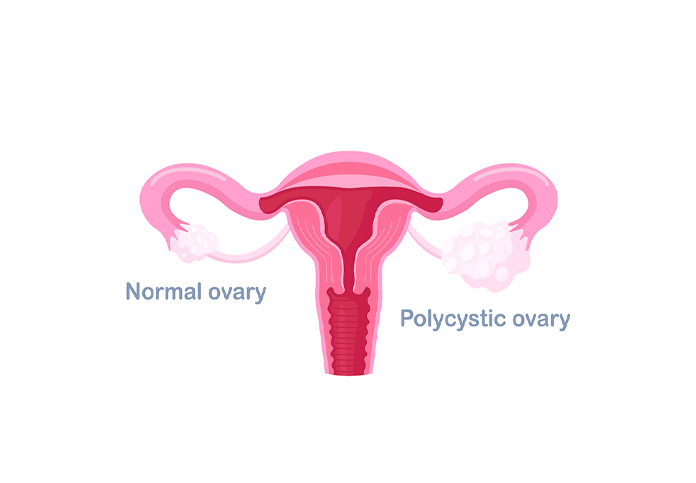
Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. It is characterized by a combination of symptoms and signs, including irregular menstrual cycles, elevated levels of male hormones (androgens), and the presence of multiple cysts on the ovaries. PCOS can impact fertility and overall health, but it is manageable with proper treatment.
Symptoms of PCOS
- Irregular Menstrual Cycles:
- Irregular or absent periods are common, often due to problems with ovulation.
- Excess Androgens:
- Elevated levels of male hormones can lead to symptoms such as excessive hair growth (hirsutism), acne, and oily skin.
- Polycystic Ovaries:
- Ovaries may have multiple small cysts (fluid-filled sacs) visible on ultrasound. These cysts are not harmful but are a marker of the condition.
- Weight Gain:
- Many women with PCOS experience weight gain or difficulty losing weight.
- Infertility:
- Difficulty getting pregnant due to irregular or absent ovulation.
- Hair Thinning:
- Scalp hair thinning or loss can occur, often due to elevated androgens.
- Skin Changes:
- Darkened skin patches (acanthosis nigricans) may appear on the neck, armpits, or groin.
- Other Symptoms:
- Mood swings, fatigue, and headaches are also reported by some women.
Causes and Risk Factors
The exact cause of PCOS is not fully understood, but several factors may contribute to its development:
- Genetics:
- PCOS may run in families, suggesting a genetic component.
- Insulin Resistance:
- Many women with PCOS have insulin resistance, where the body does not use insulin effectively, leading to higher insulin levels that can exacerbate hormonal imbalances.
- Inflammation:
- Low-grade inflammation may be present, which can affect hormone levels and ovarian function.
- Hormonal Imbalances:
- Elevated levels of androgens and irregularities in the release of hormones from the pituitary gland can impact ovulation and menstrual cycles.
- Environmental Factors:
- Lifestyle factors such as diet and exercise habits may play a role in the development and management of PCOS.
Diagnosis of PCOS
PCOS is typically diagnosed based on a combination of clinical criteria, laboratory tests, and imaging:
- Medical History and Physical Examination:
- Evaluation of symptoms, menstrual cycle patterns, and physical exam to assess for signs of hirsutism, acne, or obesity.
- Ultrasound:
- Transvaginal ultrasound can reveal the presence of multiple cysts on the ovaries.
- Blood Tests:
- Hormone levels (e.g., androgens, insulin, and glucose) are assessed to identify hormonal imbalances and rule out other conditions.
- Exclusion of Other Conditions:
- Conditions with similar symptoms, such as thyroid disorders or adrenal disorders, need to be ruled out.
Treatment for PCOS
Treatment for PCOS aims to manage symptoms, improve quality of life, and address associated health issues:
- Lifestyle Modifications:
- Diet: A balanced diet with low glycemic index foods can help manage insulin levels and weight. Eating more fruits, vegetables, and whole grains can be beneficial.
- Exercise: Regular physical activity can improve insulin sensitivity, aid in weight management, and help regulate menstrual cycles.
- Medications:Homeopathic medicines like sepia, puls,agnus are very helpful.
- Counseling and Support:
- Mental Health Support: Addressing emotional and psychological aspects related to PCOS, such as anxiety or depression, may be helpful.
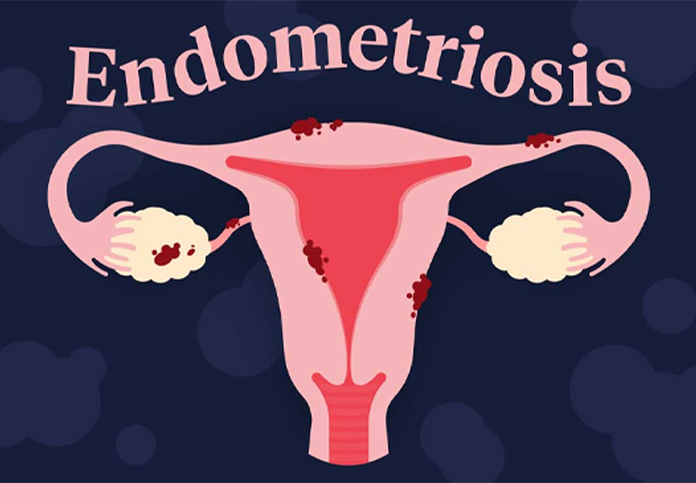
Endometriosis
Endometriosis is a chronic medical condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus. This tissue can be found on the ovaries, fallopian tubes, outer surface of the uterus, and other organs within the pelvis. It can cause pain, infertility, and other symptoms, and its severity can vary widely among individuals.
Symptoms of Endometriosis
- Pelvic Pain:
- Often described as severe menstrual cramps that may worsen over time. Pain can occur during menstruation, but also at other times of the menstrual cycle.
- Menstrual Irregularities:
- Heavy menstrual bleeding (menorrhagia) or bleeding between periods.
- Pain during Intercourse:
- Pain during or after sexual intercourse is common.
- Pain with Bowel Movements or Urination:
- Painful bowel movements or urination, especially during menstrual periods.
- Infertility:
- Endometriosis is found in 20-40% of women with infertility issues.
- Other Symptoms:
- Fatigue, diarrhea, constipation, bloating, and nausea. Some women experience symptoms that fluctuate with their menstrual cycle.
Causes and Risk Factors
The exact cause of endometriosis is not fully understood, but several theories and risk factors have been proposed:
- Retrograde Menstruation:
- Menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body.
- Embryonic Hormones:
- Estrogen exposure during puberty may transform cells in the pelvic cavity into endometrial-like cells.
- Immune System Disorders:
- Problems with the immune system might make the body unable to recognize endometrial-like tissue growing outside the uterus.
- Genetics:
- Endometriosis may run in families, suggesting a genetic predisposition.
- Environmental Factors:
- Exposure to certain environmental toxins or chemicals might contribute to the development of endometriosis.
Uterine fibroids
Uterine fibroids, also known as leiomyomas or myomas, are benign tumors that develop in the muscle tissue of the uterus. They are common, especially in women of reproductive age, and can vary in size, number, and location within the uterus.
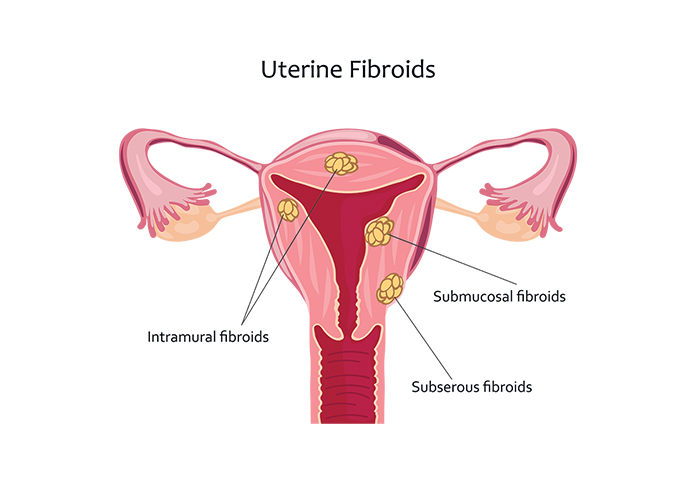
Types of Uterine Fibroids
- Intramural Fibroids:
- Found within the wall of the uterus. They are the most common type and can cause enlargement of the uterus.
- Subserosal Fibroids:
- Located on the outer surface of the uterus, projecting outward into the pelvis. They may cause pressure symptoms.
- Submucosal Fibroids:
- Situated just beneath the lining of the uterine cavity. They can cause heavy menstrual bleeding and may impact fertility.
- Pedunculated Fibroids:
- Attached to the uterus by a stalk. They can be either subserosal or submucosal and can sometimes twist or cause pain.
Symptoms of Uterine Fibroids
- Heavy Menstrual Bleeding:
- Excessive bleeding during menstruation (menorrhagia) or bleeding between periods.
- Pelvic Pain or Pressure:
- Discomfort or a feeling of fullness in the pelvic region. Large fibroids can press on nearby organs.
- Frequent Urination:
- Fibroids pressing on the bladder can cause increased urinary frequency or urgency.
- Painful Intercourse:
- Discomfort during or after sexual intercourse.
- Back Pain:
- Lower back pain due to pressure from large fibroids.
- Constipation:
- Pressure on the rectum can lead to difficulty with bowel movements.
- Enlarged Abdomen:
- A noticeable increase in the size of the abdomen or a feeling of abdominal fullness.
- Infertility:
- Fibroids, particularly submucosal ones, can interfere with implantation and pregnancy.
Causes and Risk Factors
The exact cause of uterine fibroids is not known, but several factors may influence their development:
- Hormones:
- Estrogen and progesterone may promote the growth of fibroids. Fibroids often shrink after menopause when hormone levels decrease.
- Genetics:
- Family history of fibroids may increase the risk. Certain genetic changes may be associated with their development.
- Age:
- Fibroids are more common in women in their 30s and 40s.
- Ethnicity:
- African-American women are more likely to develop fibroids and may experience more severe symptoms.
- Lifestyle Factors:
- Obesity and a sedentary lifestyle may increase the risk of developing fibroids.
Diagnosis of Uterine Fibroids
- Pelvic Ultrasound:
- Transabdominal or transvaginal ultrasound to visualize the fibroids and assess their size and location.
- Hysterosonography:
- An ultrasound procedure where saline is injected into the uterus to better visualize submucosal fibroids.
- Hysteroscopy:
- A procedure where a thin, flexible scope is inserted through the vagina and cervix to view the inside of the uterus.
- Magnetic Resonance Imaging (MRI):
- Provides detailed images of the uterus and fibroids, helping to assess their size and location, especially if surgery is being considered.
- Laparoscopy:
- A minimally invasive surgical procedure to visualize and possibly remove fibroids.
