Musculoskeletal System
Understanding Musculoskeletal System Problems: Causes, Types, and Treatments
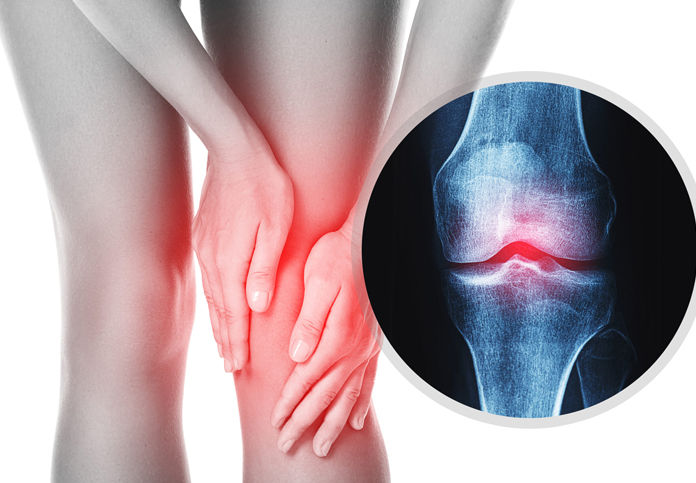
Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis, characterized by the gradual breakdown of cartilage in the joints. Cartilage is the smooth, slippery tissue that covers the ends of bones and helps joints move smoothly. In osteoarthritis, this cartilage deteriorates, leading to pain, stiffness, and reduced mobility in the affected joints. It can affect any joint but most commonly impacts the knees, hips, hands, and spine.
Symptoms:
- Joint Pain: Pain in the affected joint(s) during or after movement.
- Stiffness: Joint stiffness, especially in the morning or after periods of inactivity.
- Loss of Flexibility: Decreased range of motion in the affected joint(s).
- Swelling: The affected joint may become swollen due to inflammation.
- Grating Sensation: A feeling or sound of bone rubbing against bone, often accompanied by a clicking or cracking noise.
- Bone Spurs: Extra bits of bone, known as osteophytes, may form around the affected joint.
Causes and Risk Factors:
- Age: The risk of developing osteoarthritis increases with age, as the cartilage naturally wears down over time.
- Joint Injury or Overuse: Previous joint injuries or repetitive stress on a joint (e.g., from a job or sports) can increase the risk.
- Genetics: A family history of osteoarthritis can make you more susceptible.
- Obesity: Excess weight puts additional stress on weight-bearing joints, particularly the knees and hips, increasing the risk of OA.
- Bone Deformities: Some people are born with defective cartilage or malformed joints, which can increase the likelihood of OA.
- Other Diseases: Conditions like diabetes, rheumatoid arthritis, or metabolic disorders can contribute to the development of osteoarthritis.
Diagnosis:
- Medical History and Physical Exam: The doctor will ask about symptoms, perform a physical examination, and assess the joint's range of motion.
- X-rays: Can reveal joint space narrowing, bone spurs, and other changes typical of osteoarthritis.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the joint's cartilage, tendons, and ligaments, which can help diagnose early-stage OA or rule out other conditions.
- Joint Fluid Analysis: A sample of fluid from the affected joint can be tested to help rule out other types of arthritis or joint disorders.
Treatment:
- Lifestyle Changes:
- Weight Management: Losing weight can reduce stress on weight-bearing joints and alleviate symptoms.
- Exercise: Low-impact exercises like swimming, cycling, and walking can strengthen the muscles around the joints, improve flexibility, and reduce pain.
- Physical Therapy: A physical therapist can provide exercises and techniques to improve joint function and reduce pain.
- Medications:Homeopathic medicines like rhus tox , bryonia and arnica ,puls are really helpful.
- Assistive Devices:
- Braces or Shoe Inserts: These can help support the joint and reduce pain during movement.
- Canes or Walkers: Using a cane or walker can take pressure off painful joints, especially in the hips and knees.
Prevention and Management:
- Maintain a Healthy Weight: Keeping a healthy weight can reduce stress on joints and lower the risk of developing OA.
- Stay Active: Regular, low-impact exercise can keep joints flexible and strengthen the muscles that support them.
- Protect Your Joints: Avoid joint injuries by using proper techniques during activities and wearing protective gear when needed.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and healthy fats can help reduce inflammation and support overall joint health.
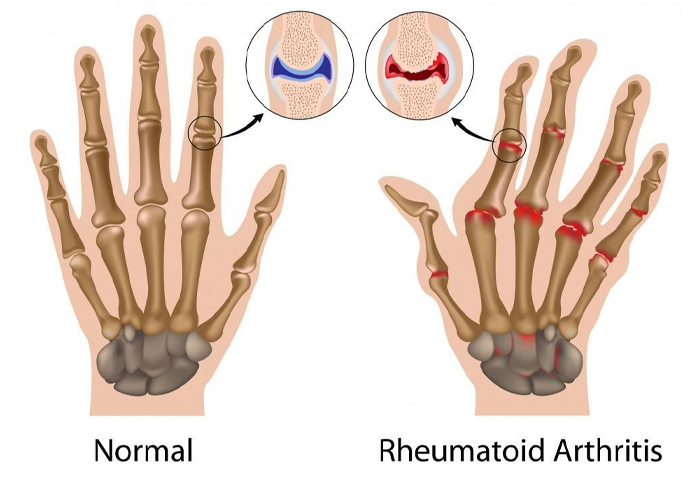
Rheumatoid Arthritis (RA)
is a chronic autoimmune disorder that primarily affects the joints, causing inflammation, pain, swelling, and eventually joint damage. Unlike osteoarthritis, which is caused by wear and tear, RA occurs when the immune system mistakenly attacks the body's own tissues, particularly the synovium, the lining of the membranes that surround the joints. RA can affect other organs and systems in the body as well.
Causes and Risk Factors:
- Autoimmune Reaction: The exact cause of RA is not known, but it is believed to involve a combination of genetic and environmental factors. The immune system attacks the synovium, leading to inflammation and thickening of the tissue, which can damage the cartilage and bones within the joint.
- Genetics: Certain genetic markers, particularly HLA-DR4, are associated with a higher risk of developing RA.
- Gender: RA is more common in women than men.
- Age: While RA can occur at any age, it most commonly begins between the ages of 30 and 60.
- Smoking: Smoking increases the risk of developing RA and can make the disease more severe.
- Obesity: Excess weight can contribute to the development and progression of RA.
Symptoms:
- Joint Pain and Swelling: The small joints of the hands, wrists, and feet are often the first affected. The pain is usually symmetrical, meaning it occurs on both sides of the body.
- Morning Stiffness: Stiffness in the joints, especially in the morning or after periods of inactivity, is a common symptom.
- Fatigue: Many people with RA experience chronic fatigue and a general feeling of malaise.
- Joint Warmth and Redness: Inflamed joints may feel warm to the touch and appear red.
- Joint Deformity: Over time, chronic inflammation can lead to joint deformity and loss of function.
- Systemic Symptoms: RA can also cause symptoms beyond the joints, such as fever, weight loss, anemia, and inflammation of the lungs, heart, and eyes.
Diagnosis:
- Medical History and Physical Exam: A doctor will assess the symptoms, including the pattern and duration of joint pain, and examine the joints for signs of inflammation.
- Blood Tests: Certain blood tests can help diagnose RA, including:
- Rheumatoid Factor (RF): An antibody found in about 70-80% of people with RA.
- Anti-Cyclic Citrullinated Peptide (anti-CCP) Antibodies: More specific for RA and can help confirm the diagnosis.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These tests measure inflammation levels in the body.
- Imaging Tests: X-rays, ultrasound, or MRI scans can show joint damage, erosion, and inflammation in the early stages of the disease.
Treatment:
Exercise: Regular, gentle exercise can improve joint flexibility and reduce stiffness. Physical therapy can help maintain muscle strength and joint function. homeopathic medicines like rhus tox, actea spicata, caulophyllum are very helpful.
Gout
Gout is a form of inflammatory arthritis caused by the accumulation of uric acid crystals in the joints, leading to sudden and severe pain, swelling, and redness. It most commonly affects the big toe but can impact other joints, such as the ankles, knees, and wrists.
Symptoms
- Intense joint pain, especially in the big toe (often occurring at night or early morning)
- Swelling, redness, and warmth in the affected joint
- Limited range of motion due to pain
- Sudden flare-ups that can last days or weeks, followed by periods with no symptoms

Causes
- High uric acid levels (hyperuricemia): Uric acid is a waste product that is normally excreted through urine. When the body produces too much uric acid or fails to excrete enough, it can build up and form sharp crystals in the joints.
- Diet: Consuming foods high in purines (found in red meat, organ meats, shellfish, and alcohol) can raise uric acid levels.
- Medications: Diuretics (water pills), low-dose aspirin, and some chemotherapy drugs may increase the risk of gout.
- Health conditions: Obesity, high blood pressure, kidney disease, and metabolic syndrome are associated with higher risks of gout.
Treatment
- Medications: homeopathic medicines like colchicum,rhododendron,benzoic acid are few top most remedies
- Lifestyle changes:
- Avoiding foods high in purines (e.g., red meat, alcohol)
- Staying hydrated
- Maintaining a healthy weight
- Regular exercise
- Managing flare-ups:
- Rest the affected joint
- Use ice packs to reduce swelling
- Stay hydrated
Back pain
Back pain is a common condition that can range from a mild, temporary ache to severe, chronic discomfort. It can affect any part of the back, but the lower back is most frequently involved due to its support of the upper body and involvement in movement.
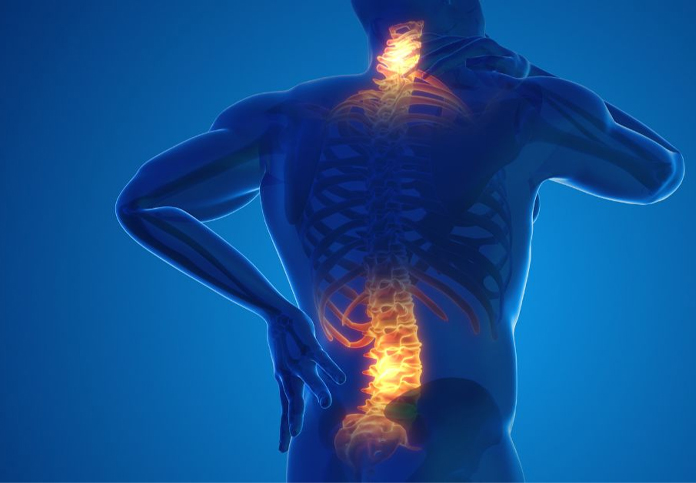
Types of Back Pain
- Acute back pain: Lasts a few days to weeks, usually caused by an injury or overuse.
- Chronic back pain: Lasts for more than three months, may result from an underlying condition or develop over time.
Causes of Back Pain
- Muscle or ligament strain: Lifting heavy objects, sudden awkward movements, or poor posture can strain muscles or ligaments in the back.
- Herniated or slipped discs: The soft material inside a disc can bulge or rupture, pressing on nearby nerves and causing pain.
- Degenerative disc disease: Discs between the vertebrae lose cushioning over time, leading to pain.
- Arthritis: Osteoarthritis in the spine can lead to the narrowing of the space around the spinal cord (spinal stenosis).
- Sciatica: Compression or irritation of the sciatic nerve, leading to pain radiating from the lower back down the leg.
- Skeletal irregularities: Conditions like scoliosis (a sideways curvature of the spine) can cause pain if the spine is not properly aligned.
- Osteoporosis: Weak, brittle bones can lead to fractures in the spine.
- Infections or tumors: Rarely, infections or tumors in the spine may cause pain.
Symptoms
- Muscle ache or tightness
- Stabbing or shooting pain
- Pain that radiates down the leg (often in cases of sciatica)
- Limited flexibility or range of motion
- Pain that worsens with bending, lifting, standing, or walking
Treatment
- Medications:homeopathic medicines like arnica , rhus tox, bryonia are very helpful.
- Physical Therapy:
- Stretching and strengthening exercises to improve posture and support the back
- Heat or cold therapy
- Massage or manual therapy
- Lifestyle Changes:
- Maintaining proper posture
- Regular exercise (especially core strengthening exercises)
- Avoiding heavy lifting or learning proper lifting techniques
- Maintaining a healthy weight to reduce strain on the back
Sciatica
Sciatica refers to pain that radiates along the path of the sciatic nerve, which runs from the lower back, through the hips and buttocks, and down each leg. It typically affects only one side of the body and can range from mild discomfort to severe pain.
Symptoms of Sciatica
- Pain: A sharp or burning pain that radiates from the lower back down the leg, sometimes as far as the foot.
- Numbness or tingling: “Pins and needles” sensation in the affected leg or foot.
- Weakness: Muscle weakness in the leg or foot, making walking or standing difficult.
- Worsening pain with movement: Coughing, sneezing, or sitting for long periods may aggravate symptoms.
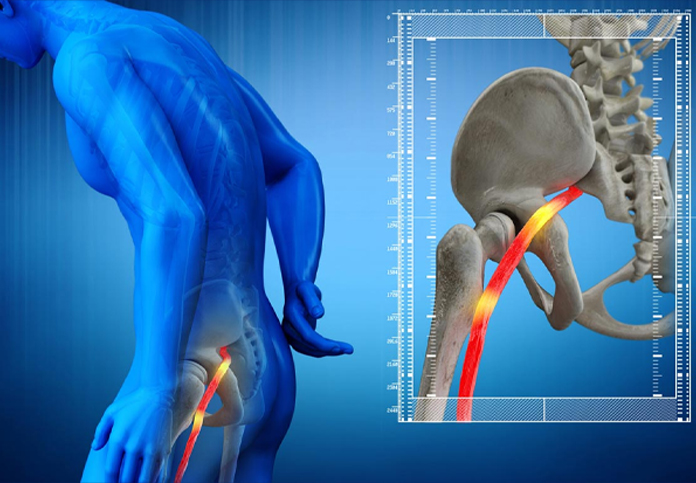
Causes of Sciatica
- Herniated or slipped disc: This is the most common cause. A disc in the spine can bulge or rupture, pressing on the sciatic nerve.
- Spinal stenosis: Narrowing of the spinal canal can compress nerves, including the sciatic nerve.
- Piriformis syndrome: The piriformis muscle in the buttock can irritate or compress the sciatic nerve.
- Spondylolisthesis: A condition where one vertebra slips forward over another, pinching the sciatic nerve.
- Injury: Trauma to the lower back or pelvis may damage the sciatic nerve.
- Degenerative disc disease: Aging-related wear and tear on spinal discs can cause nerve compression.
Treatment: Homeopathic medicines like colocynth and mag phos are very helpful.
Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a type of chronic inflammatory arthritis that primarily affects the spine, causing pain, stiffness, and, over time, the fusion of vertebrae. This can lead to a loss of flexibility and a forward-stooped posture. It can also affect other joints, tendons, and ligaments, and in severe cases, impact the eyes, heart, and lungs.
Symptoms
- Chronic back pain: Stiffness: Fusion of vertebrae: FatigueOther joints affected:.
- Inflammation in other areas: Some patients may experience uveitis (eye inflammation), heart problems, or difficulty breathing due to reduced lung function.
- Spinal fusion: Heart and lung issues: AS can cause inflammation in the heart and may reduce lung capacity.
- Eye inflammation (uveitis): Causes pain, light sensitivity, and blurred vision.
Causes
The exact cause of ankylosing spondylitis is unknown, but it is believed to involve a combination of genetic and environmental factors. One key genetic marker, HLA-B27, is strongly associated with AS, though not everyone who carries this gene develops the condition.
Lumbar Spondylitis
Lumbar spondylitis refers to inflammation in the lumbar (lower back) region of the spine, leading to pain, stiffness, and limited mobility. It is part of a broader category of spinal arthritis, often related to spondyloarthritis, a group of inflammatory diseases that affect the spine and other joints.
Causes
- Degenerative changes: Often associated with wear and tear on the spine (e.g., osteoarthritis).
- Autoimmune conditions: Inflammatory disorders like ankylosing spondylitis can lead to lumbar spondylitis.
- Infections: Rarely, infections like tuberculosis can cause inflammation in the spine.
- Injury: Trauma to the lumbar spine may lead to inflammation and chronic back problems.

Symptoms
- Lower back pain: Pain in the lumbar region that can worsen after periods of inactivity or in the morning.
- Stiffness: Difficulty bending or moving the lower back, particularly after rest.
- Radiating pain: The pain may extend into the buttocks, thighs, or legs (sciatica-like symptoms).
- Limited mobility: Reduced ability to move or bend the lower back.
- Muscle spasms: Muscles surrounding the inflamed area may spasm, causing additional pain.
Diagnosis
- Physical examination: A doctor may assess for tenderness, range of motion, and signs of nerve involvement.
- Imaging tests: X-rays, MRI, or CT scans can reveal inflammation, degeneration, or other structural abnormalities in the lumbar spine.
- Blood tests: Inflammatory markers like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) may be elevated in cases of inflammatory spondylitis.
Treatment
- Medications:homeopathic medicines like arnica,rhus tox, bryonia are very helpful .
- Physical Therapy:
- Exercises to improve flexibility, strength, and posture.
- Stretching routines to reduce stiffness.
- Manual therapy, such as spinal manipulation, may help alleviate discomfort.
- Lifestyle Changes:
- Exercise: Regular low-impact activities like walking, swimming, or yoga can improve flexibility and reduce symptoms.
- Posture correction: Maintaining good posture during daily activities can help reduce pressure on the lower spine.
- Weight management: Maintaining a healthy weight can alleviate strain on the lumbar region.
